The story of Dr. Henry Judah Heimlich
Hello there!
This text is a translation of this one on Steemit, which itself comes from an article posted on zestedesavoir.com, a french association which promotes access to free knowledge.
I apologize in advance for the eventual translation mistakes.
We often hear about the Heimlich maneuver in first aid trainings, but it's rare that we talk about Heimlich itself. This is what is propose to you today: discover the story of Henry Judah Heimlich, the inventor of the maneuver that bears his name, but not only.
As a matter of fact, Henry Judah Heimlich is the inventor of the most acclaimed method today to rescue sufferers from suffocation. But he didn't do only that, and that's what we're going to see here.
No medical knowledge is required to read this text.
Early career
Born on 3 February 1920 in Wilmington, Delaware in the United-States, Heimlich obtain his doctorate of medicine in 1943 in the Weill Medical College, a medical school of the New-York state.
He will have some success early in his career. In 1945, while he is stationed in China in the US-Navy, he finds a cure for trachoma by mixing sulfadiazine, an antibiotic used especially against toxoplasmosis, and shaving foam. Trachoma is a bacterial infection caused by chlamydia that causes serious vision problems up to total blindness.
In the 50's, he specializes in thoracic surgery and then exercises in operating rooms.
The Heimlich valve
It is in 1962 that Heimlich meet his first great success with the invention of a non-return valve which bears his name: the Heimlich valve. But before to explain how it works, I have to introduce what a pneumothorax is.
When the upper part of the body undergoes a violent shock (a fall, a high-speed collision, etc), a rib may punctunre one of the lungs. This can also happen in case of perforating wound (typically: a bullet wound). The lung will then let out the air at each inspiration. That air will accumulate in the pleura (the space normally occupied by the lungs, which is therefore empty) and will compress the lung, which will make inspiration more difficult, as if you breathe with too tight belt. At each inspiration, more air will escape into the pleura, making even more difficult the next inspiration. This phenomenon can rapidly end with a suffocation. That is what is called a pneumothorax.
It may also happen that it is not air but blood that escapes into the pleura (for example in case of internal bleeding), it is then a hemothorax. The consequences are the same, except that we must additionally consider the loss of blood.
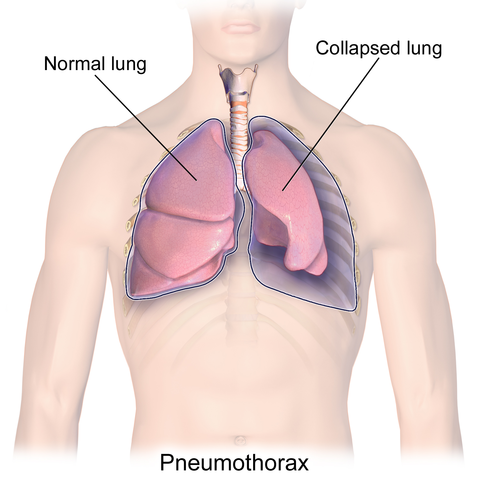
-> Illustration of a pneumothorax. We see the pleural space of the left lung being filled with air. Source.
When the lung-diaphragm assembly is at rest, there is a very low negative pressure inside the pleura : -3 mmHg (millimeters of mercury, the most used unit of pressure in medicine), or -0.4 kPa. At the inspiration, this pressure goes to -6 mmHg (or -0.8 kPa). So, there is a negative pressure between the lungs and the outside air, which creates an "aspiration". In case of perforation, this negative pressure therefore "disappears".
So, the problem is: how to get the air or the blood drained from the pleural space without the outside air comes in because of this negative pressure?
This is where the Heimlich's invention comes in. It is made of plastic tube with two connectors. Inside, one of them if connected to a flexible rubber sleeve. By connecting this to a pipe connected to the pleural space, and the other to a pump, we can aspire the content without there being a return at each inspiration.
It can be something else than a pump: any device producing a vacuum suits. The "Vacuum" fittings found in hospital rooms can be used for this purpose.
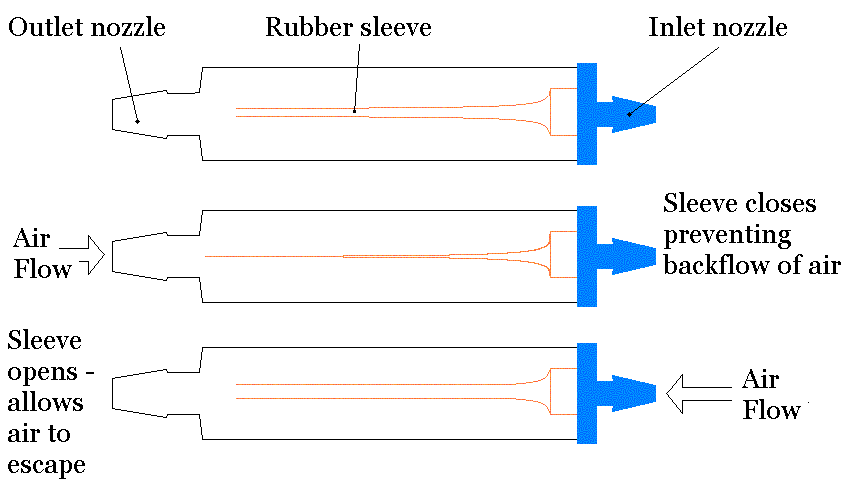
-> Schema of a Heimlich valve. Source.
In particular, this valve was used extensively to treat soldiers who were victims of gunshot wounds during the Vietnam War, and it is still used today to drain pneumo and haemothorax.
The Heimlich maneuver
It is in June 1974 that Heimlich publishes the articles which will definitely make him famous. At that time, choking was the sixth leading cause of death in the United States, and if doctors have a few ways to treat it, their effectiveness is not always there. Some recommend hitting in the back, others trying to catch the obstructing object with the fingers. Some even attempting to push the body further obstructing the trachea so that it blocks only one of the two lungs, but this maneuver is often fatal.
So, it is in the Journal of Emergency Medicine that Heimlich choose to publish an article named "Pop Goes the Cafe Coronary", where he proposes to expel the obstructive object by exerting a strong pressure upwards, near the stomach, in order to reproduce the effect of a violent cough. However, to be effective, this pressure must be very strong. In fact, try to lift the victim by the stomach. Nausea is therefore not uncommon after such a maneuver.
At this article release, his colleagues are skeptical. In particular, they fear that this may harm the internal organs and that it is difficult for the public to learn. In order to prove its maneuver's efficiency, Heimlich publishes its recommendations in public journals to have concrete feedbacks. Although debatable, this approach paid off. As soon as the June 19, the Seattle Post-Intelligencer journal reported that a resident of Washington succeeded in saving the life of a neighbor by this method. Returns of this kind multiplied, and so this method was adopted.
Entry in the references
On 1976, the American first aid organizations officially introduce the Heimlich maneuver in their references. This should be done only after attempting to give five vigorous strokes to the victim's back. This recommendation was abolished in 1985 and then restored by the American Red Cross in 2006. As often in first aid, the recommendations evolved into a saw to date.
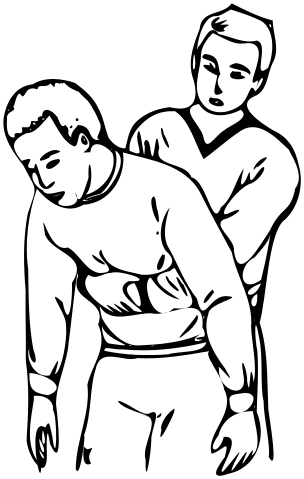
-> Illustration of the Heimlich maneuver. Source.
A person who chokes is easily spotted. He/She...
- holds his hands to his neck and has an open mouth;
- is agitated;
- can not speak, cough or breath.
To reproduce this maneuver, put yourself behind the victim, and join your fists in front of his stomach, one hand surrounding the other in order to have as much force as possible. Then, apply pressure to the back (towards you) and upwards to lift the victim by its stomach.
Attention, if the victim coughs, it's a partial chocking. In this case, do not try this maneuver. Just encourage the victim to cough and help her to position herself forward or to the side. You can (and should) of course call emergency services if this is not enough.
Today (in 2017), in America, the recommendations are as follows (Source).
- Ask the victim if she is choking to rule out a partial obstruction or other respiratory problem. The victim should not be able to answer, she is holding her hands to her neck and has her mouth open.
- Give five vigorous strokes on its back.
- In case of failure, try Heimlich's maneuver.
- If the victim loses consciousness, begin a cardiac massage.
Then, call for help (112 in Europe, 911 in America).
In 2003, a former colleague of Heimlich, Edward Patrick, claimed to be the uncredited co-creator of this maneuver. However, he could not prove what he said.
All the good things…
Family
Since June 4, 1951, Dr. Heimlich is married to Jane Murray. In 1981, the latter co-wrote the book Homeopathic Medicine At Home, where she gives homeopathic advices to treat small injuries (which is rather ironic when one knows that the inventor of homeopathy, Samuel Hahnemann, was opposed to allopathic medicine, that is to say the one practiced by Heimlich). They had four children. One of them, Peter, had conflicting relationships with his father, accusing him of "scientific fraud" because of its controversial theories. His father proposed, for example, to use his famous maneuver on asthmatics or victims of drowning, to which the entire medical community opposed. He also appears to have illegally conducted experiments on HIV-positive patients in Ethiopia.
In 2014, Heimlich published a brief named Heimlich's Maneuvers: My Seventy Years Of Lifesaving Innovation.
Prolepsis. We are now on May 23, 2016.
The doctor Henry Judah Heimlich is now 96 and is in a retirement home in Cincinnati, Ohio. At noon, burgers are on the menu. Suddenly, a women, Patty Ris, chokes with a piece of meat. A man gets up and practice a maneuver that now bears his name. Heimlich has for the last time, personally saved a life. He had already practiced this maneuver thirteen years before, saving a man from suffocation in a restaurant, although this intervention was much less mediated.

-> Screenshot from the BBC's website.
Let's move forward in time one last time.
We are now on December 17, in a room of the Christ Hospital. This is the end of the road for Dr. Heimlich, who suffered a heart attack on December 12 at his home in Hyde Park. He died at the age of 96. In 2009, the New York Times estimated that 100,000 people saved thanks to its famous maneuver in the United States alone.
In all American restaurants, there are posters explaining how to maneuver Heimlich.

-> Portrait of Dr. Henry Judah Heimlich. Source.
Conclusion
Thanks for reading me ! Before closing this article, I would like to thank all those who read it again and who contributed to its improvement during its original publication on Zeste de Savoir, as well as you, dear reader, for having followed me here.
Licence
This article is published under license « Creative Commons By-SA 4.0 rezemika ». The licenses of the images are indicated in their sources.
Sources (sorry, many are in french)
- Henry J. Heimlich on Wikipédia
- Pneumothorax on Wikipédia
- Unisciel : Une pression négative est présente dans la cavité pleurale (in French)
- Journal JIM : Longtemps à la manœuvre (in French)
- BBC : Heimlich: Still saving lives at 83
- A Heimlich in every plot
- Digital Journal : Inventor of the Heimlich maneuver discredited by his own son
- New York Times : Dr. Henry J. Heimlich, Famous for Antichoking Technique, Dies at 96