Chronic Heart Failure | Medications & Treatments
Chronic Heart Failure | Medications & Treatments

During my last post, I covered the background, some statistics, and the general pathophysiology of heart failure. This post will be a continuation of my last post, and will cover some of the most commonly utilized medications and treatments for patients with heart failure.
The cornerstone of heart failure treatments are aimed at the two main neurohormonal pathyways as discussed previously, which are the renin-angiotensin-aldosterone system (commonly referred to as RAAS) and the sympathetic nervous system (commonly abbreviated as SNS). Therefore, in naturally makes sense that the most commonly used drugs in the treatment of heart failure include: angiotensin converting enzyme inhibitors (commonly referred to as ACEI) or angiotensin receptor antagonist (commonly referred to as ARBs), neprilysin inhibitors (ARNI), Beta-Blockers and loop diuretics. All of these classes of medications work on either one or both of the main neurohormonal pathways discussed previously, which we will examine in more depth here.
Loop Diuretics
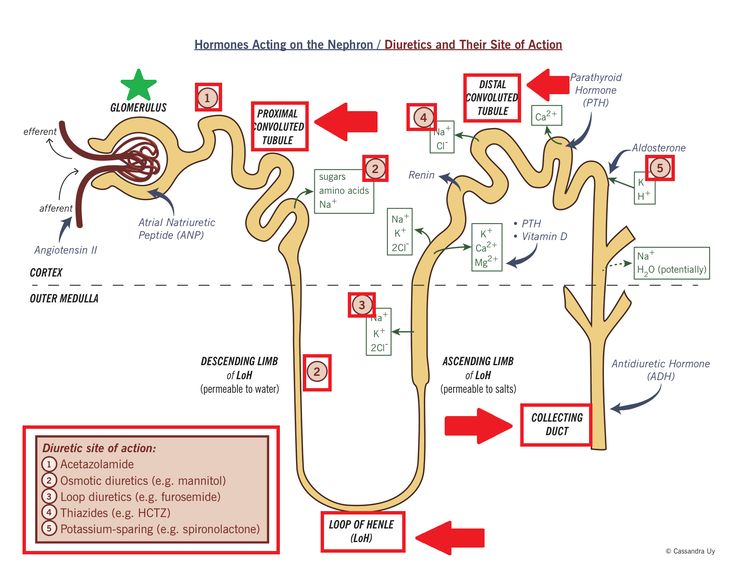
Loop diuretics are used to decrease fluid volume, which decreases edema (or water retention) making it easier for the heart to pump. Loop Diuretics work by blocking sodium and chloride reabsorption in the thick ascending loop of henle, which causes interference with the chloride-binding co-transport system. This can be seen in the image below. Consequently, this increases the amount of sodium, potassium, chloride, magnesium, and water that are excreted by the kidneys. As a result patients usually experience less lung congestion and water retention in their legs and helps to restore their body back to their “dry weight” or to a euvolemic state.
Although loop diuretics have not been shown to provide any survival benefit for patients with heart failure, most patients will require them for control of their systems. However care must be taken both by the patients themselves and by healthcare professionals in order to not cause over diuresis, which can lead to hypotension and kidney injury. This is why the lowest effective dose of a diuretic should always be used.
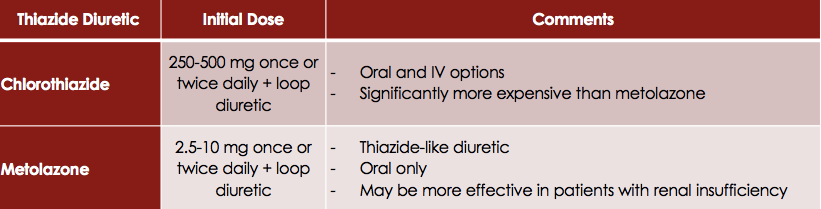
In the case where patients start to develop resistance or the response to the loop diuretic is poor, a combination of a thiazide-type diuretic in addition to a loop diuretic can be useful.
ACEI Inhibitors and Angiotensin Receptor Blockers
Like we learned in the last posting, ACE Inhibitors block the conversion of angiotensin I to angiotensin II resulting in decreased vasoconstriction and decreased aldosterone secretion. ACEI also block the degradation of bradykinin, which is thought to contribute to the vasodilatory effects and also cause one of the most common side effect of ACE inhibitors, coughing.
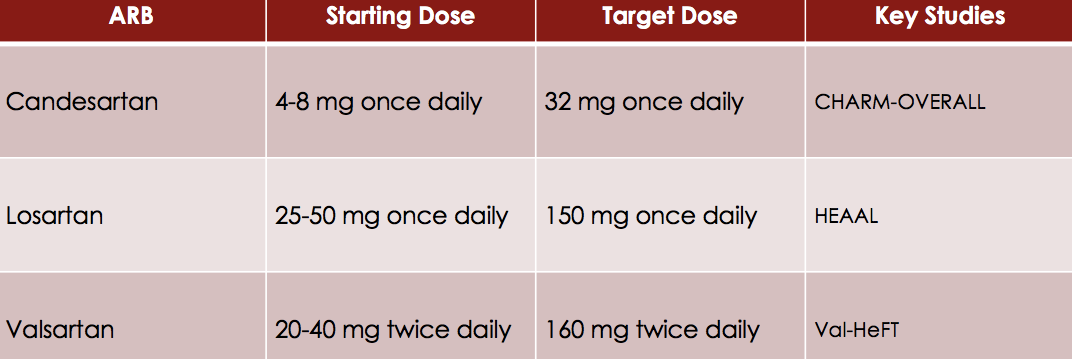
ARBs on the other hand, block angiotensin II from binding to the angiotensin II receptor. Overall, this class of medications cause decreases in RAAS activation resulting in decreased preload and afterload. Thereby, reducing the amount of cardiac remodeling, which improves the left ventricular function and improves heart failure. For this reason, it should come as no surprise that both ACE inhibitors and ARBs provide both a mortality benefit and morbidity benefit in patients with heart failure. This is also why ACE inhibitors (an ARBs if patients are not able to tolerate ACE inhibitors) are indicated for all patients with heart failure, regardless of their symptoms.
According to the American Heart Association guideline ACE inhibitors are recommended for all patients with heart failure with a reduced ejection fraction due to their beneficial effects on morbidity and mortality. ARBs on the other hand are recommended as second line agents for patients who cannot tolerate ACE inhibitors.
Of note, caution should be advised in patients with hypotension (or Blood pressures less than 80 mmHg), elevated serum creatinine (SCr > 3 mg/dL), bilateral renal artery stenosis, elevated potassium (K > 5 mEq/L).
In addition, some contraindications to ACEI and ARBs include a history of angioedema and/or pregnancy. The most common adverse events with these agents include hypotension, renal insufficiency, angioedema and hyperkalemia.
Beta-Blockers
Beta-adrenergic receptor antagonists (or beta-blockers), block the effects of catecholamines (such as epinephrine and norepinephrine) at the beta-1 and beta-2 adrenergic receptors. Beta-blockers therefore decrease vasoconstriction, improve cardiac function, and decrease morbidity and mortality. Overall, these agents are recommended for all HF patients. However, unlike ACEI or ARBs, Beta-Blockers do not exhibit a class effect. Meaning not all beta-blockers are the same for the treatment of heart failure. Only bisoprolol, carvedilol and metoprolol succinate are recommended for the treatment of heart failure in the guidelines and literature.
Beta-blockers should be used with caution in patients with reactive airway disease, bradycardia (HR<55 beats/min), hypotension (SBP<80 mmHg), recurrent hypoglycemia, and PVD. In addition, use of these agents is contraindicated in patients with persistent asthma/active bronchospasm or persistent bradycardia. The most commonly reported adverse effects with these agents include: bradycardia, hypotension, dizziness/fatigue (especially w/dose initiation or titration).
Aldosterone Receptor Antagonist
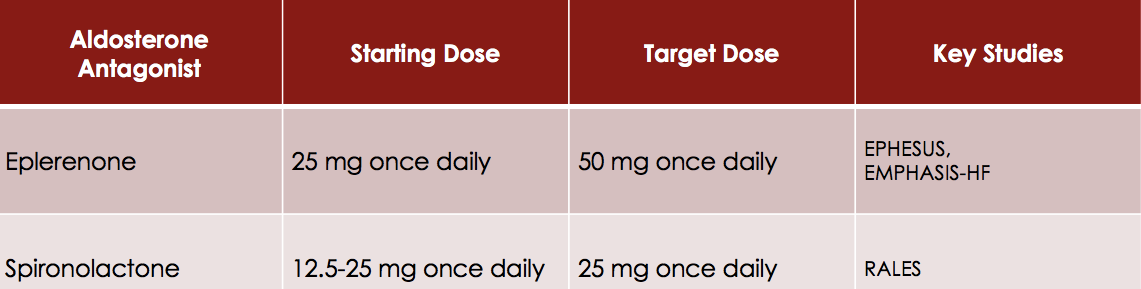
Aldosterone is a mineralocorticoid that causes sodium and water retention, with receptors in the kidneys, as well as on the heart brain, vasculature, adipose tissue and immune cells. Aldosterone receptor antagonist (ARAs) compete with aldosterone at the site of the receptor in the distal convoluted tubule and the collecting ducts within the kidney. Spironolactone is a non-selective ARA (also blocks androgen), while Eplerenone is a selective ARA that does not exhibit endocrine side effects. Overall, ARAs reduce sodium and water retention, cardiac remodeling (especially myocardial fibrosis) and the risk of sudden cardiac death. ARAs therefore reduce morbidity and mortality and should be added to standard therapy in patients with NHYA class II-IV heart failure.
The most common adverse effects associated with spironolactone and Eplerenone is hyperkalemia, which requires close monitoring and occurs more often during dose initiation and/or titration. In addition, since spironolactone is a non-selective mineralocorticoid antagonist it can also cause gynecomastia/breast pain. This side effects is not seen however with Eplerenone since this agent is more selective.
Hydralazine/Nitrates
Hydralazine is a direct arterial vasodilator which decreases afterload. Nitrates on the other hand increase the availability of nitric oxide which causes venous vasodilation and decreases preload. Hydralazine also decreases the development of nitrate tachyphylaxis (tolerance). The combination, BiDil, improves the survival of heart failure patients. Therefore, this combination is used as an alternative treatment for patients who cannot tolerate ACEI or ARBs due to poor renal function, angioedema, or hyperkalemia. BiDil is also indicated in African American patients with NYHA class III – IV patients who are symptomatic despite optimal treatments with ACEI and beta-blockers.
Although Hydralazine and other oral nitrates such as Isosorbide denigrate and Isosorbide mononitrate can be used by themselves to treat hypertension, they have not been shown to affect HF outcomes. However, these medications are still sometimes used in clinical practice. In addition the most common adverse effects reported with the use of these medications include: headache (especially with nitrate), dizziness, and GI complaints.
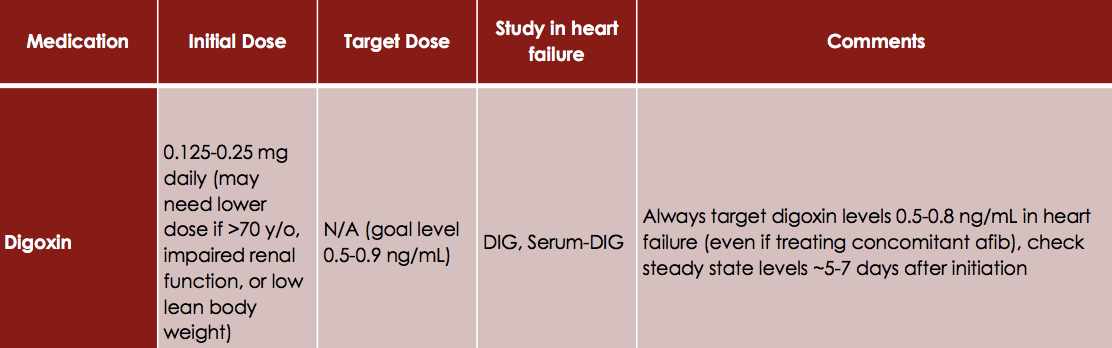
Digoxin
Digoxin inhibits the Na/K ATPase pump which results in a positive inotropic effect (increases cardiac output). It also exerts a parasympathetic effect which provides a negative chronotropic effect (decreases heart rate). Digoxin is added in patients with symptomatic heart failure despite receiving standard treatments with ACEI (or ARB) and Beta-Blockers. Although digoxin improves symptoms of heart failure it does not provide any mortality benefit but it does help reduce the rate of hospitalizations, and improves patients quality of life.
For Questions with any of the information presented here within or if you have any questions about heart failure in general, please drop a comment below and I'd be happy to answer them for you.





Very helpful post resteeming.
Thank you for your support and resteeming my post. Its great appreciated :)
You compiled this information very well, it’s nice to read other healthcare professionals blogs about health! Thanks for your informative posts!
Thank you @alcarson for your support! I agree, hoping we can grow the healthcare community together here on steemit!
Interesting read thanks @tspink hope one never has to use drugs such as these, always good to know they are available and what they do.
I couldn’t agree more. I’m currently working in a heart failure clinic at the moment and it’s amazing to see how many people have heart failure. For those with heart failure tho. these medications really are helping to save & prolong their lives!
@originalworks
Interesting, learnt lots of new things! Thanks for writing.
Thank you, glad you enjoyed it!
Thanks for the info
Got here from Kryptonia followed and upvoted but not listed as one of your followers on Kryptonia so no task reward :(
Thank you for the support @princesave I’ll have to take a look into it on kryptonia. I don’t believe you should have been able to complete the task without first being a follower tho.
#kryptonia