How a specific commensal skin bacterium might protect us against skin cancer
At first it might sound not so obvious that a bacterium could provide protection against tumour cells or have an anti-cancer effect. However, more and more evidence is provided that certain bacteria have the ability to target cancer cells and destroy them. A few years ago I even did some own experiments on this issue. I researched the effect of virulent bacterial strains (e.g. Salmonella) and symbioflor bacteria (e.g. E. coli) on cervical cancer cells (HeLa). Quite interestingly, both virulent and non-virulent strains killed most of the tumour cells albeit the efficiency of virulent strains was slightly greater. Because this was a relatively short research project I forgot about this exciting topic until now when I found this fascinating paper published in the journal Science. Researchers could show that a bacterium on our skin (Staphylococcus epidermis) has a protective effect against skin cancer in mice (Nakatsuji et al., 2018).
Besides Staphylococcus epidermidis (S. epidermis) Staphylococcus hominis is another staphylococcal species living on our skin (Kloos and Musselwhite, 1975). Quite interestingly, other staphylococcal strains are present on our skin during a skin disease e.g. atopic dermatitis. In this context, S. aureus was found to be predominant (Abeck and Mempel, 1998). Remarkably, research indicated an interaction of the skin microbes with the epidermis in a way that it can alter the skin ecology (Sanford and Gallo, 2013).
Staphylococcus epidermidis
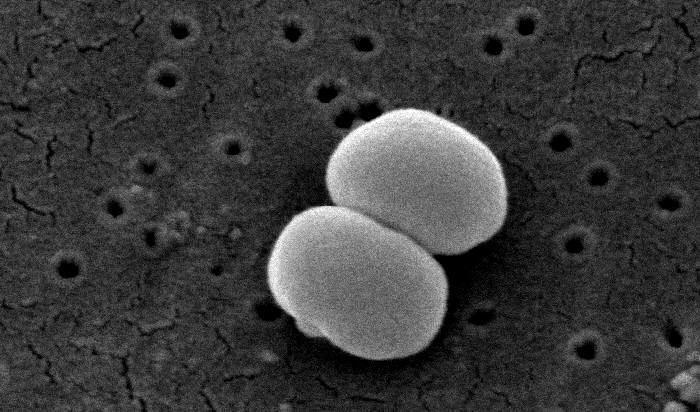
Source
Although some research has been done, the exact mechanism of how skin bacteria influence the host is barely understood. However, it was demonstrated that certain staphylococcal strains could protect the host against harmful infections. Specific strains of Staphylococcus can produce proteins that interact with so called host antimicrobial peptides (AMPs) that together confer protection against pathogenic bacteria or other infections (Cogen et al., 2010;Nakatsuji et al., 2017).
One example is the production of phenol-soluble modulins (PSMs) by S. epidermidis which were found to directly kill pathogens such as group A streptococcus (GAS) and S. aureus (Cogen et al., 2010;Cogen et al., 2010).
Furthermore, S. epidermidis was also shown to have additional effects that benefit the skin’s immune function. It was demonstrated to increase the production of T-cells (Laborel-Préneron et al., 2015), reduce inflammation (Lai et al., 2009) and to enhance the generation of AMPs by the host (Lai et al., 2010). In total, current research provides evidence for a highly important and essential interaction between the skin microbiome and the host.
As previously mentioned, researchers at the University of California, San Diego could demonstrate a certain strain of S. epidermidis to selectively prevent the proliferation of specific tumour cell lines without affecting the growth of normal cells (Nakatsuji et al., 2018). Initially they found S. epidermidis to produce a molecule called 6-N-hydroxyaminopurine (6-HAP). Nakatsuji and colleagues could show that 6-HAP impedes the thymine-adenine base pairing, thus preventing a complete DNA synthesis. Remarkably, they only observed this inhibition in tumour lines. Primary cell lines (primary keratinocytes) were not affected by 6-HAP. This was the first hint indicating an anti-cancer effect of S. epidermidis and its 6-HAP.
Furthermore, they identified the reason for the selective proliferation inhibition. The resistance of primary cells against 6-HAP is due to the generation of mitochondrial amidoxime reducing components (mARC1 and mARC2). These proteins were found to be strongly expressed in primary cell lines but not in tumour cells.
Following this, the effect of 6-HAP in mice was tested in regard to its systemic toxicity. Mice were intravenously injected with 6-HAP over a time frame of two weeks. They could show that 6-HAP did not induce a systemic toxicity nor alterations in liver function and blood count. Additionally, they tested 6-HAP on mice with melanoma. Strikingly, 6-HAP distinctly inhibited the growth of skin cancer in mice.
Skin melanoma

Source
Based on this, Nakatsuji and colleagues suggested an effect of S. epidermidis against skin cancer development. Due to the presence of these microbes on the skin surface this might be very likely. To confirm this hypothesis they used a ultraviolet carcinogenesis model. In principle, hairless mice were treated with UV-B irradiation and colonized with a strain of S. epidermidis producing 6-HAP or a control strain (that does not produce 6-HAP). The control mice showed the assumed tumour formation while mice colonized with 6-HAP generating S. epidermidis displayed a reduced number of tumours. Therefore, this indicated a potential anti-cancer effect of 6-HAP and S. epidermidis, thus suggesting a possible role in the treatment of skin cancer.
Although this seems very promising, it has to be pointed out that human trials are definitely required to confirm 6-HAP conferring protection against skin cancer. Nevertheless, these findings might provide an explanation why some people never develop skin cancer. This might be due to the presence of this specific strain of S. epidermidis on their skin that is capable of producing 6-HAP, thus preventing the development of skin cancer.
What are your thoughts on using bacteria as a cancer treatment? I would love to hear your ideas!